Pioneer of Modern Hip Arthroplasty
Total Hip Replacement had been aptly regarded as “Operation of
the Century”.
The pioneering work by Sir John Charnley (29 August 1911 – 5 August 1982), the
Father of
Modern Hip Arthroplasty
revolutionised the management of patients crippled with hip arthritis in the early 1960s.
Despite the initial disheartening outcome with PTFE, the advent of
UHMWPE
& PMMA
(Bone Cement) coupled with principle of “Low Frictional
Torque” paved
the way
upon which the foundation of modern hip arthroplasty is laid. Subsequent innovation,
technological advances, surgical refinement have greatly impacted the survivorship
of implants & expanded the spectrum of this surgery.
Total Hip Replacement has emerged as a Standout Procedure
aiming
at alleviation of disabling pain, stiffness, correction of existing limb length discrepancy
thereby
restoring mobility & transforming Quality of Life of patients with
End
Stage Hip Arthritis.
However, it is imperative to emphasise that Total Hip Replacement is a
major surgery.
Your consultant will provide guidance regarding the potential benefits of the
surgery,
but ultimately, the decision to proceed rests with you. It is essential to ensure that your
expectations regarding the outcome are realistic and that you have a clear understanding of
the
entire process involved. The intention of this article is to furnish you with sufficient
information
to make an informed decision.

Sir John Charnley
What Are the Most Common Causes of Damage to the Hip?
Common causes of damage to the hip leading to Total Hip Replacement Surgery are as
follows:
1. Avascular Necrosis:
Results from disruption of blood supply of femoral
head. Lack of blood supply causes death of bone tissues, collapse of bone & ultimately
secondary osteoarthritis of the hip.
Common causes are:
- Alcohol abuse & smoking
- Steroid abuse
- Post traumatic (Neck femur fracture/hip dislocation)
- Idiopathic
- Post Covid AVN
- Sickle cell anemia/Gaucher's disease
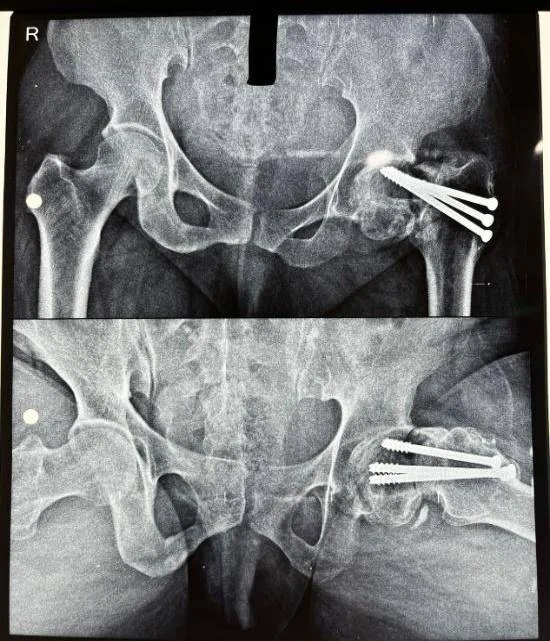
2. Hip Fractures:
Hip fractures contribute to a substantial proportion of
Arthroplasty surgery with the spectrum ranging from Modular Bipolar Hip Arthroplasty to
Primary
Total Hip Arthroplasty.
Common indications are:
- Neck femur fracture
- Basicervical trochanteric fracture
- Acetabular fracture with hip arthritis
Failed hip fixation / Implant Cut out can also be effectively salvaged with Revision Total
Hip
Arthroplasty.
3. Osteoarthritis:
By far the commonest indication of Total Hip Replacement.
Essentially due to degeneration of articular cartilage of the hip joint resulting from age
related
or secondary to any hip pathology.
4. Inflammatory Arthritis:
Genetically predisposed autoimmune disorders like
Ankylosing Spondylitis, Rheumatoid Arthritis causes inflammation of the hip joints with
consequent
arthritis & osteoporosis. Eventually the progression of disease results in significant pain,
stiffness & incapacitation of day-to-day activity thus necessitating Total Hip Replacement.
5. Developmental Dysplasia:
Essentially a developmental anomaly with distortion of
normal hip anatomy leading to premature hip arthritis with shortening & instability. Often
an
indication of Complex Primary Total Hip Replacement in relatively younger population.
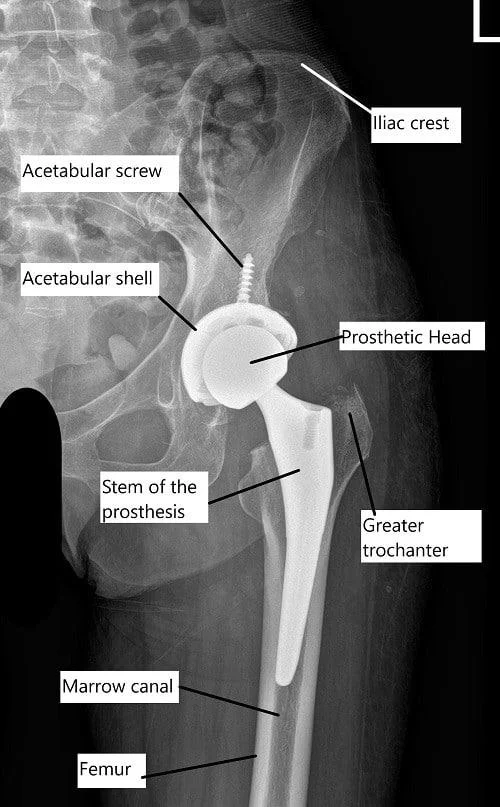
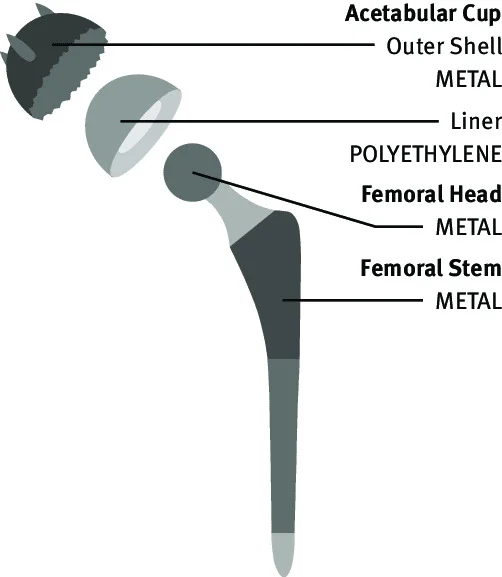
Hip Joint Prosthesis
Total Hip Replacement implants can be categorised into two broad segments:
1. Uncemented:
Both acetabular cup & femoral stem are implanted & stability is achieved through “Bone
in-growth / on-growth” over Porous coating / HA coating on surface of implant.
2. Cemented:
Both acetabular cup & femoral stem are implanted & fixed with acrylic bone cement (Palacos).
Certain situations demands flexible approach with Hybrid / Reverse Hybrid configuration
of implants.
1. Femoral Component
Stem
Cemented Stem
-
Composition: Orthinox forged SS (Exeter), cobalt chromium
(CPCS).
-
Fixation: Fixation & stability through acrylic bone cement in
the femoral shaft.
Uncemented Stem
-
Composition: Titanium Alloy (Tivanium / Beta Titanium Alloy)
-
Surface Coating: Hydroxyapatite/ Porous coating, allowing bone
growth onto its surface
Head
-
The head is attached to the neck of the stem through “Morse Taper
Locking”.
-
Composition: Metal (Co-Cr-Mo) -Oxinium (known
for its toughness and resistance to wear and corrosion) &
Ceramic (least wear rate, suitable for young, active
individuals).
2. Acetabular Component
Uncemented
-
Consists of a shell made of titanium alloy with porous coated surface, allowing
bone growth.
-
Liner: Highly cross-linked polyethylene (XLPE) &
Ceramic liners.
Cemented
-
Made of highly cross-linked polyethylene with excellent wear resistance.
-
Implanted into reamed acetabulum through fixation with bone cement.
Careful consideration is essential for implant selection, particularly for younger
individuals, as the prosthesis may require revision surgery in the future. Uncemented
Component with Ceramic Bearing may be more suitable in such cases.
Pre-Operative Evaluation
Preparation for Surgery
1. Medical Evaluation:
Medical assessment
will be conducted to evaluate your overall health.
The purpose is to
identify any existing medical comorbidity that can adversely influence with
the surgery or recovery.
Special attention needs to be focused on Comorbidities like:
Diabetes
Ischaemic Heart Disease (Prior Infarction /
Angioplasty)
Cardiac Arrhythmia (Pacemaker in situ)
Rheumatoid Arthritis
Chronic Kidney Disease
Chronic Liver Disease
2. Medications:
Inform your surgeon
about the medications you are currently taking.
The surgeon will
provide guidance on which medications should be discontinued or can be
continued before the surgery.
Special attention needs to be focused on medications like:
Anticoagulants (Clopidogrel/ Apixaban/
Ecosprin 150)
DMARD (Folitrax, Leflunomide)
Steroids
3. Pre-Operative Tests
I. Pre-Anesthetic Evaluation:
CBC & PBS, ABO /Rh Grouping
CRP, ESR
Renal Function Panel (RFT)
Liver Function Panel (LFT)
Coagulation Panel: PT, INR, BT , CT
Glycaemic Panel: FBS, PPBS, HbA1C
Serology Panel: HBsAg, Anti HCV, HIV1&2, p24
Antigen (CMIA/CLIA)
Urine R/E
Aerobic Culture of Urine
Chest X-RAY PA View
ECG 12 Leads
2-D Echocardiography
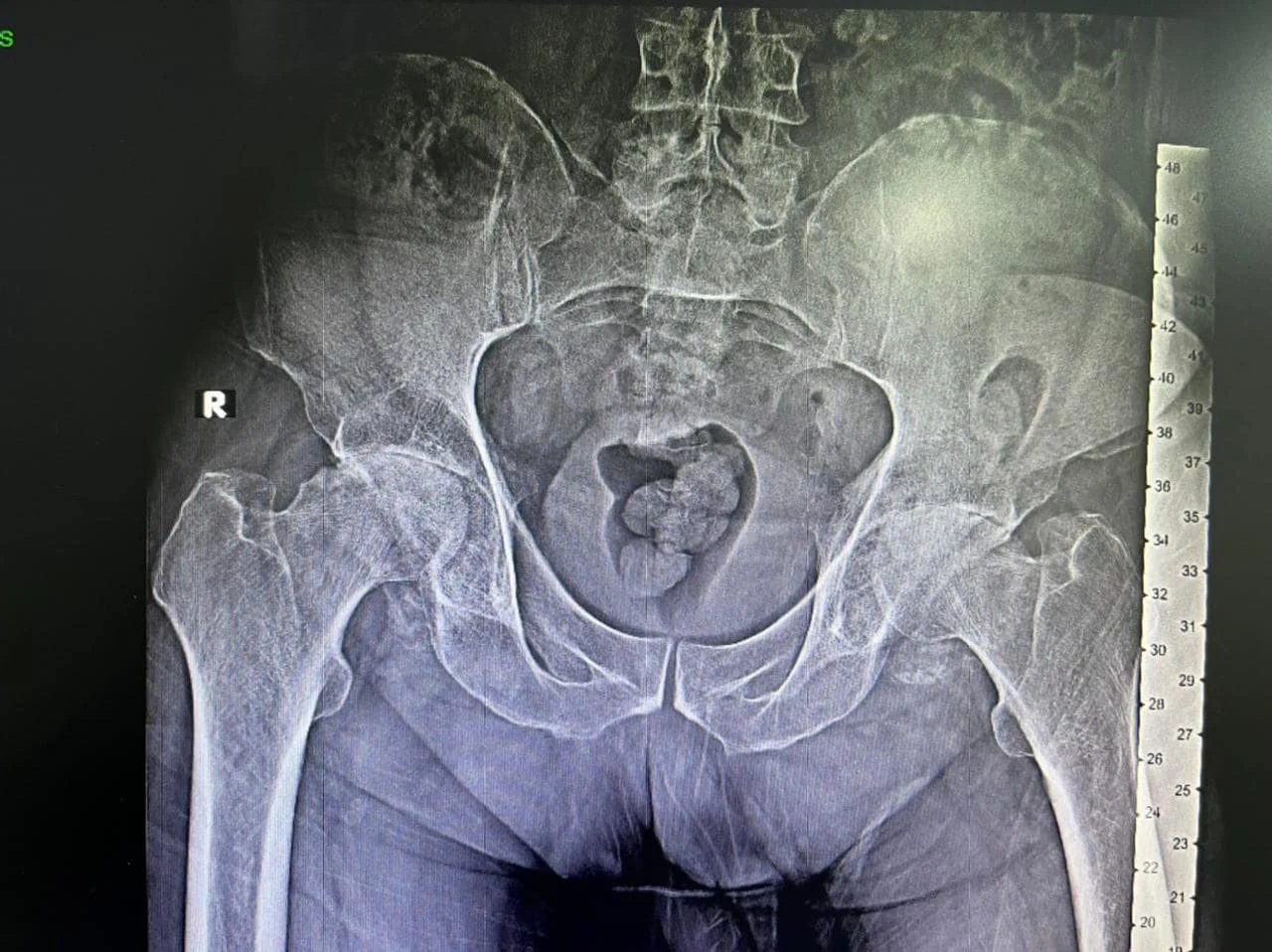
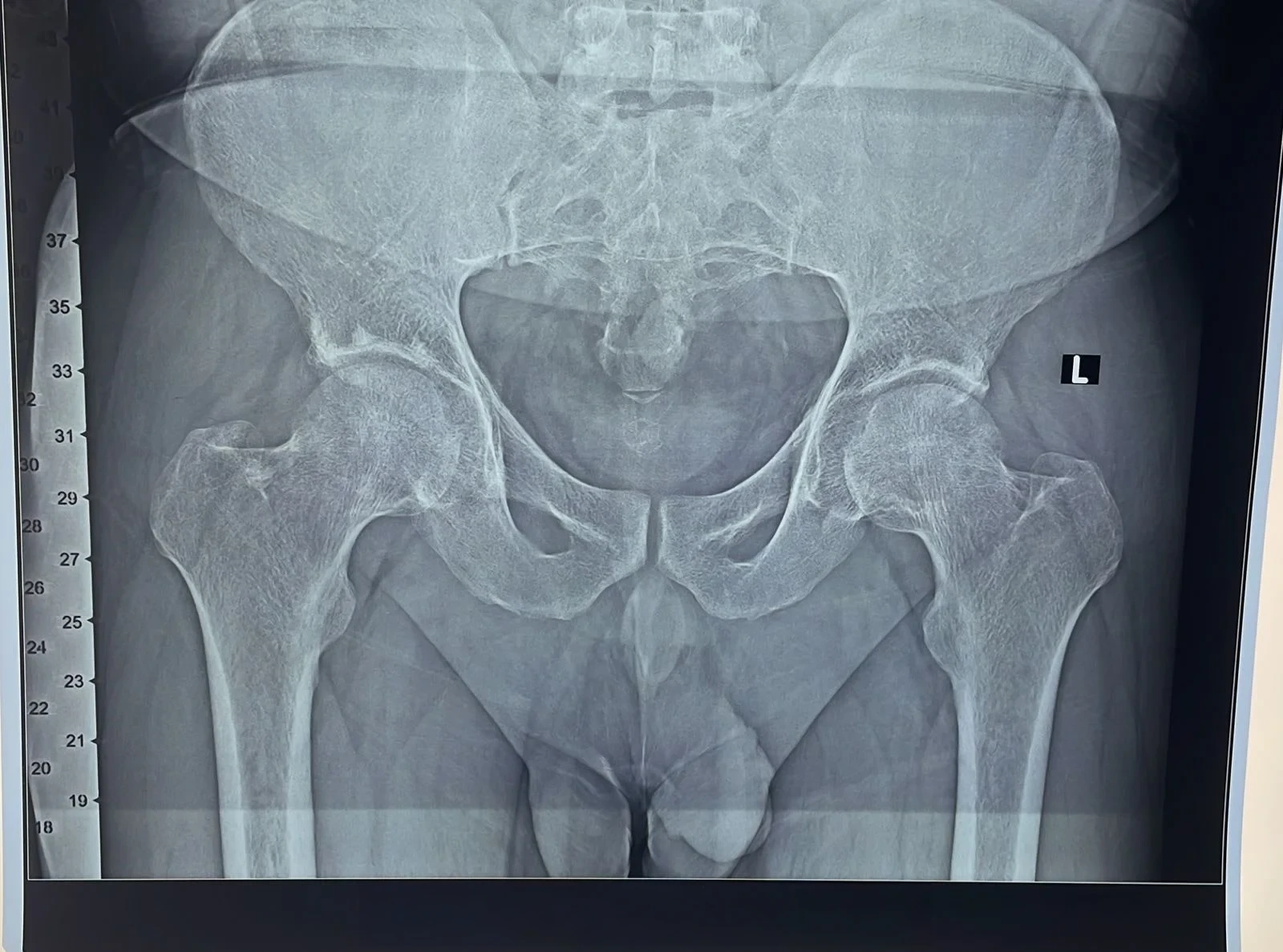
II. Pre-Operative Planning:
Digital X-Ray Pelvis with Both Hip Joint: True
Size AP
View
Digital X-Ray Hip Joint: Lat View
Digital X-Ray: Femur Whole Length with Knee Joint
(AP/Lat view)
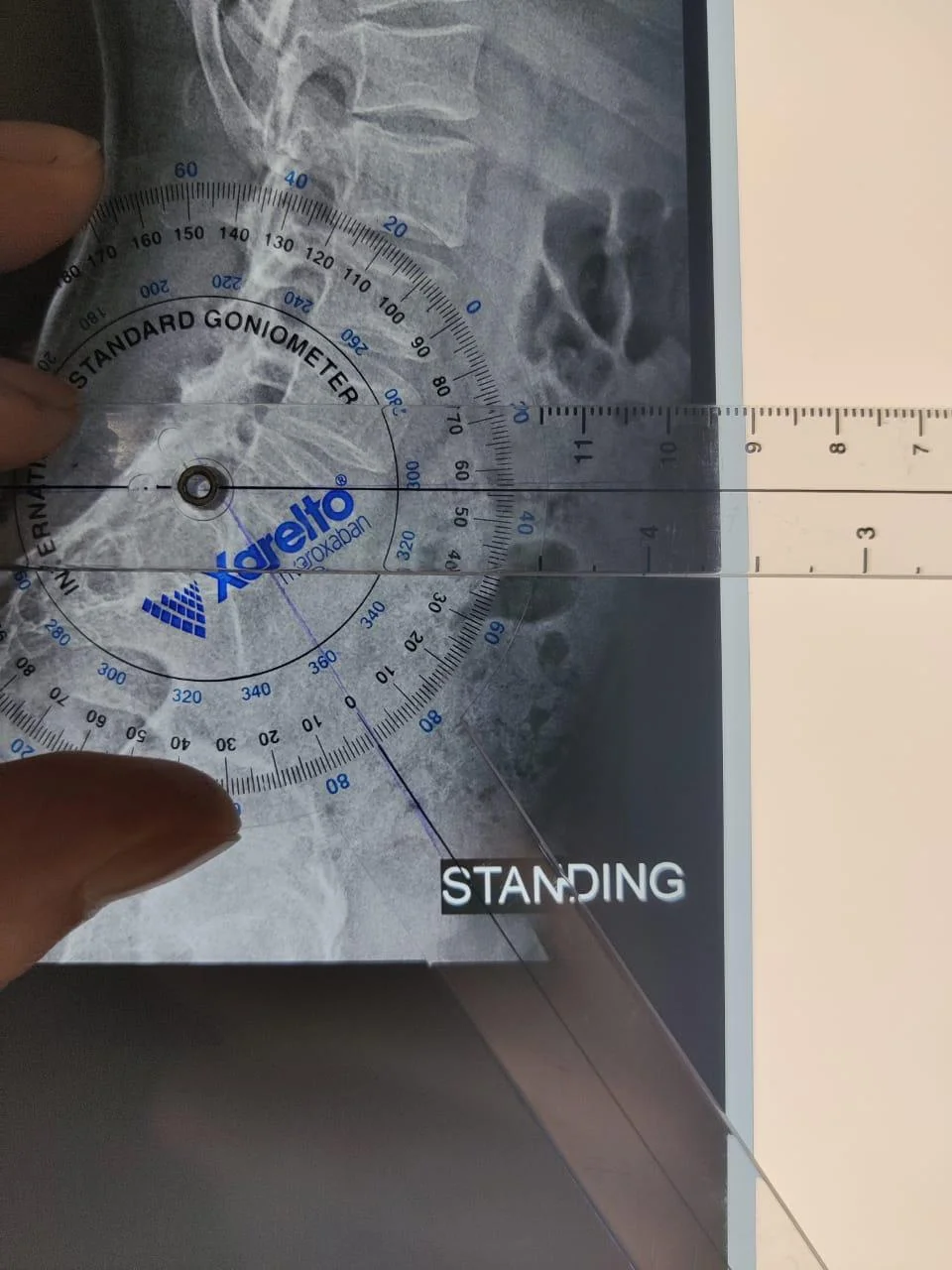
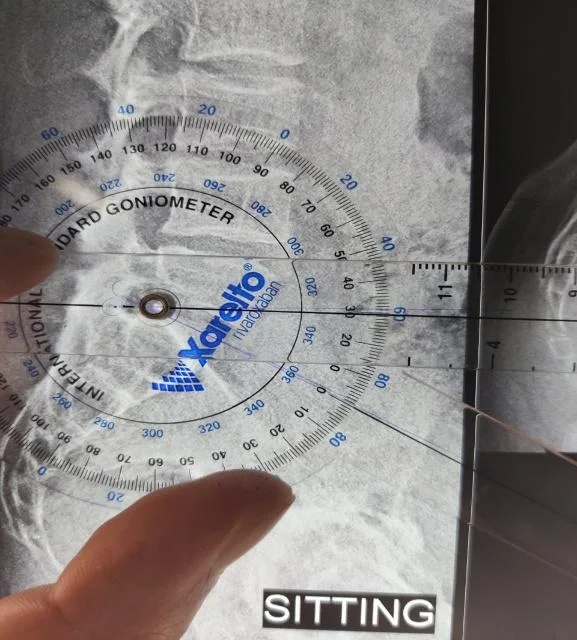
Digital X-Ray: L-S Spine Lateral View (Standing &
Sitting)
CT Scan / MRI of Hip Joint (Reserve
indication)
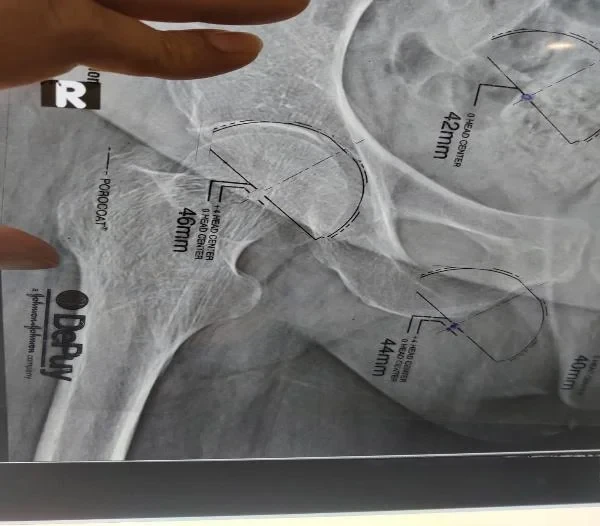
III. Pre-Op Templating :
Pre-Operative estimation of probable implant
sizes,
Offset & LLD
Anticipating any additional inventory if
required
Estimation of Sacral Slope
4. Dental Evaluation
Dental procedures can
potentially introduce bacteria into the bloodstream.
Therefore, it is
advisable to address any significant dental issues, such as tooth
extractions or periodontal work, before hip replacement
surgery.
5. Urinary Evaluation
Individuals with a
recent or frequent history of urinary infections should
consider a urological evaluation prior to hip replacement
surgery.
Older men with
prostate disease should also undergo a urologic evaluation
and treatment, if necessary, before the operation.
Financial Estimate
1. Cost Considerations
Understand the financial implications of the chosen prosthesis.
Take into account the overall cost of the procedure, including the prosthesis, hospital stay, & allied expenses.
2. Hospital Stay and Cost
Be aware of the expected duration of your hospital stay & associated costs.
Consider any potential additional expenses that may arise during your stay.
3. Mediclaim Facility
If you have mediclaim insurance coverage, contact the hospital's mediclaim department at least one week before the surgery.
Provide them with your policy documents and ensure all necessary procedures are followed.
Peri-Operative Protocol
Upon your admission to the hospital, a resident or registrar doctor will visit
you. They will conduct general evaluation & provide a brief explanation of pre
and post-operative procedures.
An Anaesthesiologist will visit you to explain the type of anesthesia to be
administered, medications that need to be discontinued, and medications to be
taken on the day of surgery. You will be instructed for NBM (to refrain from
eating or drinking) for at least 6-8 hours before the surgery.
Dr. Sanyal will visit you in the evening, explaining to you in detail about the
procedure. He will perform a final clinical evaluation & cross check his pre
operative planning. The OT timing, Implant & other relevant issues will also be
re-iterated by him.
Prior to surgery, you will be asked to bathe with Avaguard Solution on the night
before the procedure and a few hours before it, ensuring cleanliness of your
body and the surgical site.
Usually 1 -2 units of PCV are reserved prior to surgery as an exigency measure
for anticipated blood loss. Majority of patients doesn’t require post-operative
blood transfusion.
Surgical Procedure for Total Hip Replacement
1. Anesthesia
- You will be transferred to OR at the appointed hours of surgery. The anesthesia team will
establish IV access & administer IV antibiotics & other pre-anesthetic medication.
- Majority of cases of hip replacement are performed under spinal/epidural anesthesia where
patients retain their consciousness but feel numb below the waist.
- In reserved indications, general anesthesia needs to be administered.
- Choice of anesthesia is at the absolute discretion of the anesthesia team.
2. Positioning & Draping
- After the positioning is done by turning the patient to lateral decubitus & securing the
patient firmly with clamps.
- Thorough cleansing of the operative limb from flank to toes is performed using 10%
Betadine solution & 2% Sterilium.
- Draping of the operative limb is performed using Hallyard Draping Sheet, Hip U Drape, Sterile Stockinette & IOBAN.
3. Surgery
Usual duration of surgery is 90-100 mins. The surgery principally aims at precise resection of
diseased femoral head, serial reaming of acetabulum for preparation for acetabular cup & serial
broaching of femoral canal for femoral stem.
The Acetabular Cup is implanted into reamed acetabular cavity followed by placement of designated
liner (Highly Crosslinked PE/ Ceramic).
The femoral stem is implanted into broached femoral canal. Trialling is performed for judicious
selection of most appropriate size ensuring adequate restoration of offset & limb length with
assessment of stability & impingement free ROM.
Final Head size is selected & implanted onto Femoral Stem (Metal/ Ceramic/
Oxinium). After final reduction closure of soft tissue sleeve is done with
Ethibond No 5. Wound is closed in layers using absorbable sutures & skin with
staplers. Occlusive dressing applied.
3. Post Surgery
Patient will be shifted to the OR recovery room where he/she will undergo observation for another 1-2 hours. Later on the patient will be shifted to the ward.
Patients are allowed to have liquid 4 hours after surgery & semi-solid diet at night.
Hospital Stay and Recovery
Your hospital stay typically lasts 4 to 5 days.
Analgesic medications (Parenteral & Oral) will be administered appropriately weighing the existing
co-morbidity.
Day 1 After Surgery
- Transdermal analgesic skin patch will be applied.
- Ambulation with walker (PWB) under assistance from a physiotherapist.
- CBC & RFT.
Day 2 After Surgery
- Dressing change.
- Post-op x-ray.
- Continuation of physiotherapy.
Day 3 After Surgery
- Chair transfer, commode training, staircase climbing.
- Discharge on Day 3 afternoon.
How to care After Your Total Hip Replacement Surgery?
- Your surgical wound will have staples that will be removed around 14
days
post surgery.
- Sponging of body is allowed but avoid bathing till wound is healed (4-5
days
after staples removal).
- Surgical wound will be covered with occlusive dressing. Don’t change
dressing at home.
- Exercise is the most critical component of home care, particularly
during
the first 4-6 weeks post surgery.
- Daily 30-45 minutes dedicated exercise under supervision of a trained
physiotherapist.
- Strengthening of hip abductors, thigh & calf muscles to improve
endurance &
regain muscle strength.
- ROM exercises & specific activity programme.
- Use a walker for the first 1 month until you improve your balance,
flexibility & strength.
- Stairs are of particular concern. Always have someone beside you during
staircase ascend/descend. (Up with Good, Down with Bad).
- Avoid crossing your legs. Keep abduction pillow between two limbs for
the
initial 1 month.
- Do not sit on low chairs; the height of your hip joint should be higher
than
the level of your knee joint.
- Do not sit with your legs crossed.
- Opt for a commode chair.
- Minimize twisting and bending forwards.
- Continue usage of stockinettes for 1 month post surgery.
- Active ankle pump exercise.
- Oral anticoagulant (Xarelto 10 mg / Eliquis 2.5) 35 days post surgery.
- Loss of appetite & alteration of bowel habits are quite common post
surgery.
- Maintain a balanced diet with adequate protein intake to ensure proper
tissue healing & regain muscle strength.
- Ensure proper hydration by consuming ample fluids.