Total Knee Replacement is virtually a “Holy Grail” for
patients crippled with knee arthritis.
The first TKR was performed in 1968. Subsequent innovation, technological advances,
surgical refinement have greatly impacted the efficacy & spectrum of this surgery. Today
approximately 250000 TKRs are performed annually in India.
Total Knee Replacement essentially aims at alleviation of pain,
correction of deformity effectively restore mobility & thus transforming the
Quality of Life for those experiencing
severe knee pain and disability.
However, it is imperative to emphasise that Total Knee Replacement is a
major surgery.
Your healthcare consultant will provide guidance regarding the potential benefits of the
surgery, but ultimately, the decision to proceed rests with you. It is essential to
ensure that your expectations regarding the outcome are realistic and that you have a
clear understanding of the entire process involved. The intention of this article is to
furnish you with sufficient information to make an informed decision.
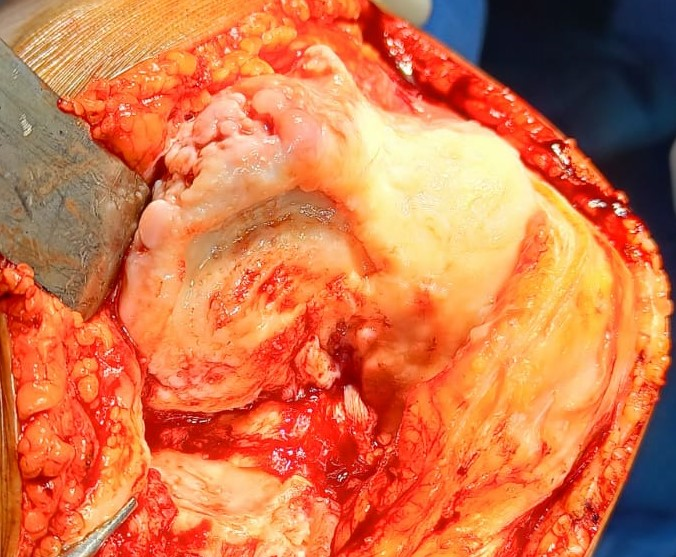
1. Osteoarthritis: By far the most common cause, resulting from the degeneration of articular cartilage. Eburnation causes friction between the bones, leading to pain, stiffness & deformity.


2. Rheumatoid arthritis: Autoimmune disease characterised by inflammation in multiple joints. It primarily affects women in their middle age (30-40yrs). Early diagnosis is of paramount importance for prevention of advanced crippling arthritis.
3. Post traumatic Arthritis/Post HTO: Intra-articular Proximal Tibia & Distal Femoral fractures can lead to secondary arthritis of knee due to chondral abrasion & associated articular cartilage damage. Appropriately indicated HTO can stall but can never prevent development of age related cartilage degeneration & subsequent arthritis.
4. Miscellaneous:
Gout & Crystalline Arthropathy
SPONK (UKR > TKR)
Haempophllic Arthropathy & PVNS
Seeking appropriate medical care and making lifestyle changes can help alleviate symptoms and improve joint health in these conditions.
Cemented Fixed Bearing TKR (PS/CR) is the Gold Standard across the globe. Factors taken into consideration for knee joint prosthesis include:
● Age & Level of Physical Activity
● Degree of Deformity
● Competence of Collateral Ligaments
● Bone defect
● Metal (Nickel) Allergy
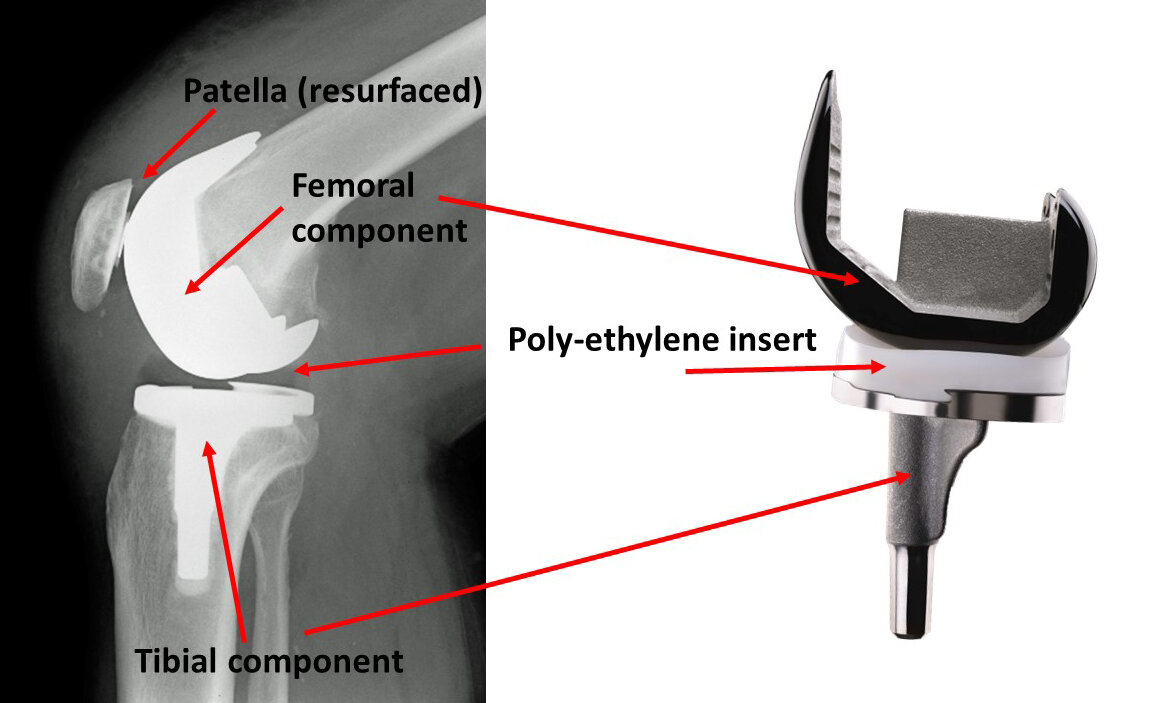
Designed & contoured for fixation in distal femur
Composition:
● Co- Cr- Mo: High strength, Corrossion resistant alloy
● Oxinium: Oxidised Zirconium exhibits exceptional wear resistance
Suitable for Younger Population & Known Nickel Allergy
Tibial Baseplate with fings/keels contoured for fixation in proximal tibia
Design: Asymmetrical (Anatomical) vs Symmetrical
Composition:
● Tivanium alloy (Ti- 6 Al-4V)
● Co- Cr- Mo
Specifically designed for fixation in tibial baseplate
Locking mechanism: Implant Specific
Radiolucent (Not Visible on X-Ray)
Composition:
● UHMWPE
● Vit E Doped UHMWPE
High Viscocity Palacos Bone Cement is most commonly used
UHMWPE with 3 peripheral lug holes for fixation in Re-surfaced Patella
● Medical assessment will be conducted to evaluate your overall health.
● The purpose is to identify any existing medical co-morbidity that can adversely influence with the surgery or recovery.
Special attention needs to be focused on Comorbidities like:
● Diabetes
● Ischaemic Heart Disease (Prior Infarction/Angioplasty)
● Cardiac Arrythmia (Pacemaker in situ)
● Chronic Kidney Disease
● Chronic Liver Disease
● Inform your surgeon about the medications you are currently taking.
● The surgeon will provide guidance on which medications should be discontinued or can be continued before the surgery.
Special attention needs to be focused on Medications like:
● Anticoagulants (Clopidogrel/Apixaban/
Ecosprin 150)
● DMARD (Folitrax, Leflunomide)
● Steroids
I. Pre-Anaesthetic Evaluation:
CBC & PBS, ABO/Rh Grouping
CRP, ESR
RENAL FUNCTION PANEL (RFT)
LIVER FUNCTION PANEL (LFT)
COAGULATION PANEL: PT, INR, BT, CT
GLYCAEMIC PANEL: FBS, PPBS, HbA1C
SEROLOGY PANEL: HBsAg, Anti HCV, HIV1&2, p24 Antigen (CMIA/CLIA)
URINE R/E
AEROBIC CULTURE OF URINE
CHEST X-RAY PA VIEW
ECG 12 LEADS
2D ECHOCARDIOGRAPHY
II. Pre Operative Planning:
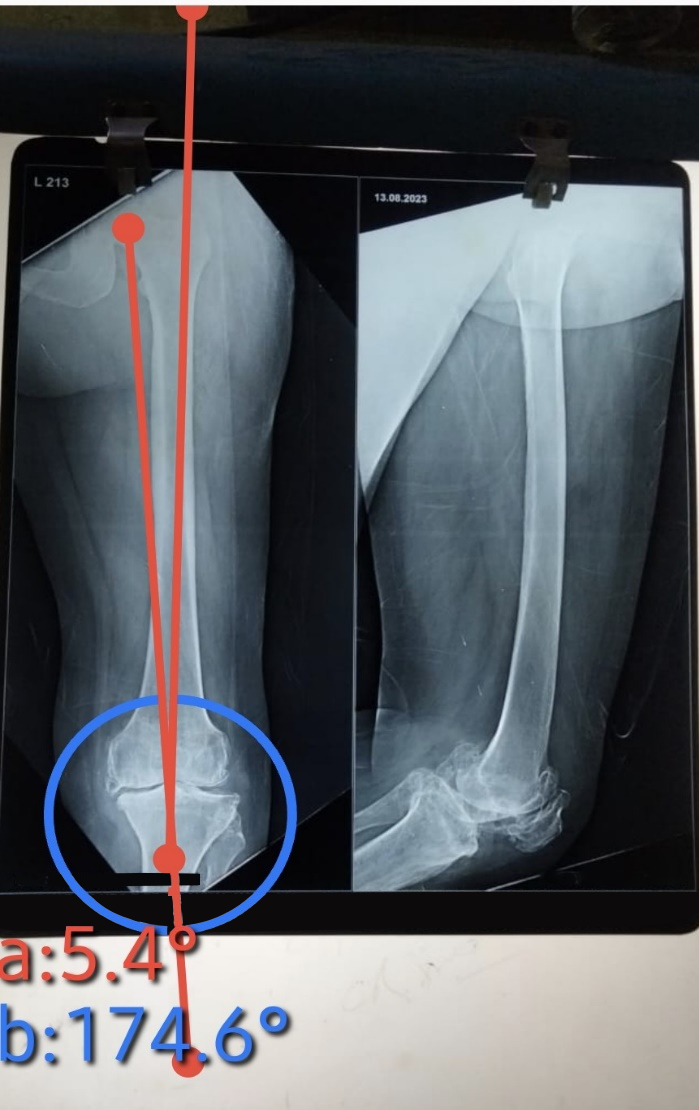
Orthoscanogram of Both Lower Limb
Digital X-Ray Knee Joint:
- AP (standing wt bearing)
- Lat view
- Axial view
Color Doppler Study of Lower Limb (Reserved Indication)

● Dental procedures can potentially introduce bacteria into the bloodstream.
● Therefore, it is advisable to address any significant dental issues, such as tooth extractions or periodontal work, before knee replacement surgery.
● Individuals with a recent or frequent history of urinary infections should consider a urological evaluation prior to knee replacement surgery.
● Older men with prostate disease should also undergo a urologic evaluation and treatment, if necessary, before the operation.
● Understand the financial implications of the chosen prosthesis.
● Take into account the overall cost of the procedure, including the prosthesis, hospital stay, & allied expenses.
● Be aware of the expected duration of your hospital stay & associated costs.
● Consider any potential additional expenses that may arise during your stay.
● If you have mediclaim insurance coverage, contact the hospital's mediclaim department at least one week before the surgery.
● Provide them with your policy documents and ensure all necessary procedures are followed.
Upon your admission to the hospital, a resident or registrar doctor will visit you. They will conduct general evaluation & provide a brief explanation of pre and post-operative procedures.
An Anaesthesiologist will visit you to explain the type of anesthesia to be administered, medications that need to be discontinued, and medications to be taken on the day of surgery. You will be instructed for NBM (to refrain from eating or drinking) for at least 6-8 hours before the surgery.
Dr. Sanyal will visit you at evening, explaining you in detail about the procedure. He will perform a final clinical evaluation & cross check his pre operative planning. The OT timing, Implant & other relevant issues will also be reiterated by him.
Prior to surgery, you will be asked to bathe with Avaguard Solution on the night before the procedure and a few hours before it, ensuring cleanliness of your body and the surgical site.
Usually 1 -2 units of PCV are reserved prior to surgery as a exigency measure for anticipated blood loss. Majority of patients do not require post operative blood transfusion.

● You will be transferred to OR at the appointed hours of surgery. The Anaesthesia team will establish IV access & administer IV Antibiotics & other pre -anaesthetic medication.
● Majority of cases of Knee Replacement are performed under Spinal/Epidural Anaesthesia where patient retain their consciousness but feel numb below waist.
● In reserved indications General Anesthesia needs to be administered. Choice of anaesthesia is absolute discretion of the Anaesthesia team.
After Anaesthesia patient positioning is done & Pneumatic Torniquet is applied over thigh of operating limb.
Thorough cleansing of operative limb from midthigh to toes is performed using 10% Betadine solution & 2% Sterilium.
Draping of operative limb is performed using Hallyard Draping Sheet, Knee O Drape & IOBAN.


Usual duration of surgery is 90-100 mins. The surgery principally aims at precise measured resection of eroded cartilage & bone of knee joint, correction of deformity, appropriate balancing of soft tissue.
The prosthesis is implanted to cut surface of distal femur & proximal tibia with specifically designated bone cement.
Cocktail infiltration is given locally intra-operatively to reduce post operative pain. Wound is closed in layers using absorbable sutures & skin with staplers.
Occlusive dressing with compression bandage & stockinettes are applied.
Patient will be shifted to OR recovery room where he/she will undergo observation for another 1-2 hours. Later on patient will be shifted to ward.
Patients are allowed to have clear fluid & liquid 4 hours after surgery & semi-solid diet at night.


You will be transferred to OR at the appointed hours of surgery. The Anaesthesia team will establish IV access & administer IV Antibiotics & other pre -anaesthetic medication.
Majority of cases of Knee Replacement are performed under Spinal/Epidural Anaesthesia where patient retain their consciousness but feel numb below waist.
In reserved indications General Anesthesia needs to be administered. Choice of anaesthesia is absolute discretion of the Anaesthesia team.

After Anaesthesia patient positioning is done & Pneumatic Torniquet is applied over thigh of operating limb.
Thorough cleansing of operative limb from midthigh to toes is performed using 10% Betadine solution & 2% Sterilium.
Draping of operative limb is performed using Hallyard Draping Sheet, Knee O Drape & IOBAN

Usual duration of surgery is 90-100 mins. The surgery principally aims at precise measured resection of eroded cartilage & bone of knee joint, correction of deformity, appropriate balancing of soft tissue.
The prosthesis is implanted to cut surface of distal femur & proximal tibia with specifically designated bone cement.
Cocktail infiltration is given locally intra operatively to reduce post operative pain. Wound is closed in layers using absorbable sutures & skin with staplers.
Occlusive dressing with compression bandage & stockinettes are applied.

Patient will be shifted to OR recovery room where he/she will undergo observation for another 1-2 hours. Later on patient will be shifted to ward.
Patients are allowed to have clear fluid & liquid 4 hours after surgery & semi-solid diet at night.
Your hospital stay typically lasts 4 to 5 days.
Analgesic medications (Parenteral & Oral) will be administered appropriately weighing the existing co morbidity.
Transdermal Analgesic skin patch will be applied.
A compression bandage which had been applied over sterile dressing will be removed.
Ambulation with walker under assistance from a physiotherapist.
CBC & RFT
Dressing is changed.
Post op x-ray.
Continuation of physiotherapy (Knee Muscle Strengthening, ROM).


Chair transfer, commode training, staircase climbing.
Discharge on Day 3 afternoon.
Your surgical wound will have staples that will be removed around 14 days post surgery.
Sponging of body is allowed but avoid bathing till wound is healed (4-5 days after staples removal).
Surgical wound will be covered with occulive dressing. Do not change dressing at home.
Exercise is the most critical component of home care, particularly during the first 4-6 weeks post surgery.
Daily 30-45 mins dedicated exercise under supervision of a trained physiotherapist.
Strengthening of thigh & calf muscle to improve endurance & regain muscle strength.
ROM exercises & specific activity programme.
Loss of apetite & alteration of bowel habits are quite common post surgery.
Maintain a balanced diet with adequate protein intake to ensure proper tissue healing & regain muscle strength.
Ensure proper hydration by consuming ample fluids.
Use walker for the first 1 month until you improve your balance, flexibility & strength.
Stairs are of particular concern. Always have someone beside you during staircase ascend/descend. (Up with Good, Down with Bad)
Continue usage of stockinettes for 1 month post surgery.
Active ankle pump exercise.
Oral anticoagulant (Xarelto 10 mg / Eliquis 2.5) 14 days post surgery.